Myelodysplastic syndrome
Myelodysplastic syndrome
Definition
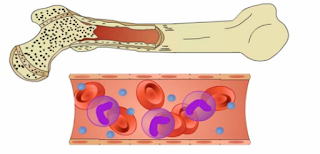
MDS is a group of diseases that affect the blood and bone marrow. Bone marrow is the soft, spongy tissue inside bones. In MDS, the blood-forming cells (stem cells) in the marrow slow down, or even stop, making the 3 types of blood cells:
Red blood cells – carry oxygen throughout the body
White blood cells – help fight infections
Platelets – help the blood clot and stop bleeding
In MDS dysfunctional blood cells fail to develop normally and enter the bloodstream. As a result, individuals with MDS have abnormally low blood cell levels (low blood counts). General symptoms associated with MDS include fatigue, dizziness, weakness, bruising and bleeding, frequent infections, and headaches. In some affected individuals, MDS may progress to life-threatening failure of the bone marrow or develop into acute leukemia. The exact cause of MDS is unknown. There are no clear risk factors but genetics and the environment may play a part.
Epidemiology
MDS occurs most commonly in older adults, with a median age at diagnosis in most series of ≥65 years and a male predominance. Onset of the disease earlier than age 50 is unusual, with the exception of treatment-induced MDS, but rare cases of MDS have been reported in children at a median age of six years. The risk of developing MDS increases with age. In one study, the annual incidence per 100,000 was estimated to be 0.5, 5.3, 15, 49, and 89 for individuals <50, 50 to 59, 60 to 69, 70 to 79, and >80 years of age, respectively.
Types
The World Health Organization divides myelodysplastic syndromes into subtypes based on the type of blood cells — red cells, white cells and platelets involved.
Myelodysplastic syndrome subtypes include:
Myelodysplastic syndrome with unilineage dysplasia: One blood cell type —white blood cells, red blood cells or platelets is low in number and appears abnormal under the microscope.
Myelodysplastic syndrome with multilineage dysplasia: In this syndrome, two or three blood cell types are abnormal.
Myelodysplastic syndrome with ring sideroblasts: This type, which has two subtypes, involves a low number of one or more blood cell types. A characteristic feature is that existing red blood cells in the bone marrow contain a ring of excess iron called ring sideroblasts.
Myelodysplastic syndrome associated with isolated del chromosome abnormality: People with this syndrome have low numbers of red blood cells, and the cells have a specific mutation in their DNA.
Myelodysplastic syndrome with excess blasts- types 1 and 2: In both these syndromes, any of the three types of blood cells — red blood cells, white blood cells or platelets might be low and appear abnormal under a microscope. Very immature blood cells (blasts) are found in the blood and bone marrow.
Myelodysplastic syndrome, unclassifiable: In this uncommon syndrome, there are reduced numbers of one of the three types of mature blood cells, and either the white blood cells or platelets look abnormal under a microscope.
Risk factors
A risk factor is anything that increases a person’s chance of developing a disease. Although risk factors often influence the development of MDS, most do not directly cause MDS. Some people with several risk factors never develop MDS, while others with no known risk factors do. However, knowing your risk factors and talking about them with your doctor may help you make more informed lifestyle and health care choices.
The following factors may raise a person’s risk of developing MDS:
Age: MDS occurs most often in people older than 60 and is less common in younger people. MDS is rare in children.
Gender: Men develop MDS more often than women.
Exposure to environmental/occupational hazards: Long-term exposure to benzene, tobacco smoke, insecticides, and other toxins may increase the risk of developing MDS.
Previous chemotherapy or radiation treatment: Approximately 20% of people who develop MDS previously received chemotherapy or radiation therapy. This type of MDS is called secondary MDS (see Subtypes and Classification).
Genetics: Most often, MDS is not inherited, meaning passed from parent to child within a family. However, some genetic changes may increase a person’s risk of developing MDS. Many of these are linked with the inherited genetic conditions listed below, with the specific genes involved when identified.
Causes
Why defects arise in the bone marrow and cause MDS in a particular person at a particular time is difficult to understand, although the effects of ageing on cell growth appears to play a major role. Any process which damages genes and leads to mutations may have a role in the development of MDS. There are also some recognised factors that may put some people at a higher risk of developing MDS:
- Ageing appears to be the most important risk factor for MDS because the risk of developing mutations increases with age
- Exposure to high levels of some environmental chemicals, especially benzene and petroleum products
- Exposure to chemicals in tobacco smoke
- People previously treated for cancer or other conditions with chemotherapy are at an increased risk of developing what is called secondary or treatment-related MDS. This accounts for less than 10% of all cases of MDS
- Previous radiation therapy, or accidental exposure to high levels of environmental irradiation
- People with certain congenital disorders such as Bloom’s Syndrome, Down’s Syndrome, Fanconi anaemia and neurofibromatosis can have unstable genes and are more at risk of developing mutations that cause MDS or cancer.
Symptoms
- A main feature of myelodysplastic syndromes (MDS) is that they cause low blood cell counts. Sometimes this is found on blood tests, even before symptoms appear. In other cases, symptoms related to shortages of one or more types of blood cells (cytopenias) are the first sign of MDS:
- Having too few red blood cells (anemia) can lead to feeling tired, dizzy, or weak, as well as shortness of breath and pale skin.
- Not having enough normal white blood cells (leukopenia), especially cells called neutrophils (neutropenia), can lead to frequent or severe infections.
- Having too few blood platelets (thrombocytopenia) can lead to easy bruising and bleeding. Some people have frequent or severe nosebleeds or bleeding from the gums.
Other symptoms can include:
- Weight loss
- Fever
- Bone pain
- Loss of appetite
These symptoms are more likely to be caused by something other than MDS. Still, if you have any of these symptoms, especially if they don’t go away or get worse over time, see your doctor so that the cause can be found and treated, if needed.
Complications
Complications of myelodysplastic syndromes include:
Anemia: Reduced numbers of red blood cells can cause anemia, which can make you feel tired.
Recurrent infections: Having too few white blood cells increases your risk of serious infections.
Bleeding that won’t stop: Lacking platelets in your blood to stop bleeding can lead to excessive bleeding.
Increased risk of cancer: Some people with myelodysplastic syndromes might eventually develop a cancer of the blood cells (leukemia).
Diagnosis and test
MDS is usually a diagnosis of exclusion and obtaining a detailed history of the patient. Physical examinations and tests are essential to rule out other conditions such as renal failure, chronic infections, aplastic anemia, medications and alcohol ingestion.
If the diagnosis is suspected clinically, further tests such as blood tests and bone marrow tests including cytogenetics are done to confirm the diagnosis.
It should be emphasized that every case should be classified according to the WHO criteria mentioned above and prognosis of each case assessed by the International Prognostic Scoring System (IPSS).
Blood tests:
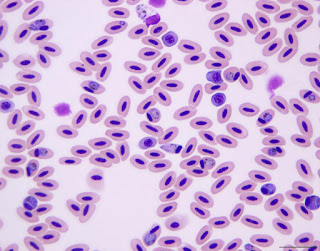
- Peripheral blood counts may show cytopenias in one or more lineages i.e. in RBC, WBC or platelets.
- Abnormal forms of red cells, white cells and platelets can be identified on a blood film examination.
- Increased numbers of immature cells or blasts may be seen in the blood film.
- Biochemical tests such as lactate dehydrogenase (LDH), ferritin, transferrin and transferrin saturation, vitamin B12 and folate concentrations, reticulocyte counts, haptoglobin, creatinine and endogenous erythropoietin (EPO) levels may help in excluding or supporting a diagnosis of MDS.
- If the diagnosis of MDS is established, LDH and ferritin levels have a prognostic value.
- Levels of EPO can help to decide whether or not to treat with erythropoietin stimulating agents.
Bone marrow tests: Bone marrow aspirate
During a bone marrow aspirate, a needle is introduced into the marrow usually on the back of the hip bone. A small amount of liquid marrow is drawn out and spread on a glass slide for microscopic analysis.
- Typically the bone marrow shows an increased number of precursor cells (hypercellularity), although it may rarely be hypocellular.
- Abnormal forms of RBC precursors include megaloblasts (abnormally large red cell precursors), and ringed sideroblasts (RBC precursors with increased iron content).
- Platelet precursors may be small (micro-megakaryocytes), mononuclear megakaryocytes, and megakaryocytes with dumbbell shaped nuclei.
- Neutrophil precursors show nuclear abnormalities. The precursors are predominantly immature precursors with a failure to mature as shown by decreased numbers of maturing forms in the marrow.
Bone marrow biopsy
Alongside a bone marrow aspirate, a piece of bone may also be removed (bone marrow biopsy) and examined to assess for any abnormality.
Bone marrow biopsy is useful when the aspirate is dry and shows scant cells (hypocellular). It is thus useful in making a diagnosis of hypoplastic or fibrotic MDS. In addition, a bone marrow biopsy may show evidence of fibrosis and carry prognostic value.
Cytogenetics
Clonal chromosomal abnormalities are noted in about 70% of the cases at diagnosis depending on the subtype and whether it is primary or secondary MDS. Even in those patients with a normal clonal karyotype at diagnosis, abnormal clones can develop during the course of the disease usually indicating a graver outcome.
Treatment
Some of the major treatments which can be performed to help patients get rid of myelodysplastic syndrome to a large extent.
Blood transfusion: blood transfusions are performed to remove and replace the deteriorated blood cells with healthy ones from patient’s body. It helps in increasing the blood count by distributing sufficient amount of oxygenated blood in a body.
Immunosuppression treatment: surgeons may use chemotherapy drugs when patients are at a greater risk of developing acute myeloid leukimea. Chemotherapy treatment can efficiently cease the abnormal cell growth and helps patient to stay in a healthy state of being.
Chemotherapy drugs: Surgeons may use chemotheraphy drugs when patients are at a greater risk of developing acute myeloid leukemia. Chemotherapy treatment can efficiently cease the abnormal cell growth and helps patient to stay in a healthy state of being.
Stem cell transplant or bone marrow transplant: Stem cell transplant procedure involves implanting new and healthy stem cells in patient’s body. Surgeons kill the abnormal cells by chemotherapy drugs or radiation treatment prior to performing this transplantation procedure. As this procedure is intensive in nature, patients should not have any chronic illness or disease. Patients with a good general health condition are considered to be ideal candidates for undergoing a bone marrow transplant.
Myelodysplastic syndrome treatment cost may vary depending on provisions of medical care center and patients requirement.
Prevention
There is no sure way to prevent myelodysplastic syndromes (MDS). But there are things you can do that might lower your risk.
- Not smoking
- Avoiding exposure to radiation or certain chemicals


Comments
Post a Comment